Justice for Henrietta Lacks
Note: Originally published as “Gerechtigkeit für Henrietta Lacks” in the German publication nd; translated by the author.
Human cell lines are an instrumental part of basic biomedical research and necessary for the development of vaccines and drugs. Compared with ordinary cells in the body, cell lines in the laboratory can divide much more often, sometimes indefinitely; they are “immortalized,” either through artificial genetic changes in the laboratory or natural mutations in the development of tumors. Anyone who conducts biomedical laboratory research is used to writing the names of the respective cell lines hundreds, thousands of times on small and large vessels and containers—in the vast majority of cases without ever having to care about their origin. Even in collections like the American Type Culture Collection (ATCC) there is sparse information about the individuals whose cells researchers around the world care for, process, and measure every day. The ATCC is one of many nonprofit institutions worldwide that protect target lines as a valuable research resource by collecting cell lines, authenticating them—i.e. checking their identity—and releasing them to researchers free of contamination.
Very special cells
The elongated shape of HeLa cells growing at the bottom of the culture vessel has been viewed through the microscope by many thousands of people working in cancer research around the world. The ATCC catalog states that the cell line HeLa “was isolated in 1951 from a cervical carcinoma derived from a 31-year-old patient,” and hints at its importance for the biomedical research community: “HeLa cells are the first immortal human cells to be grown in culture and the basis for countless significant scientific discoveries.” As the first cells that could be cultivated in the laboratory, the HeLa cell line did indeed play a central role in medical-historical milestones such as the development of the first polio vaccine and medications for diseases such as leukemia and Parkinson's.
Today, thousands of human cell lines are sold profitably by companies, collected by institutes like the ATCC, and exchanged between cooperating scientists across borders. But in 1951, the development of the HeLa cell line represented a biotechnological revolution. It also represents a blatant case of unethical treatment of test subjects, structural racism in research, and pharmaceutical company greed. Rebecca Skloot, an American science journalist, published the results of her years of research into the scandalous HeLa story in 2010, bringing attention to the case and starting the fight for compensation for the descendants of Henrietta Lacks.
Structural racism
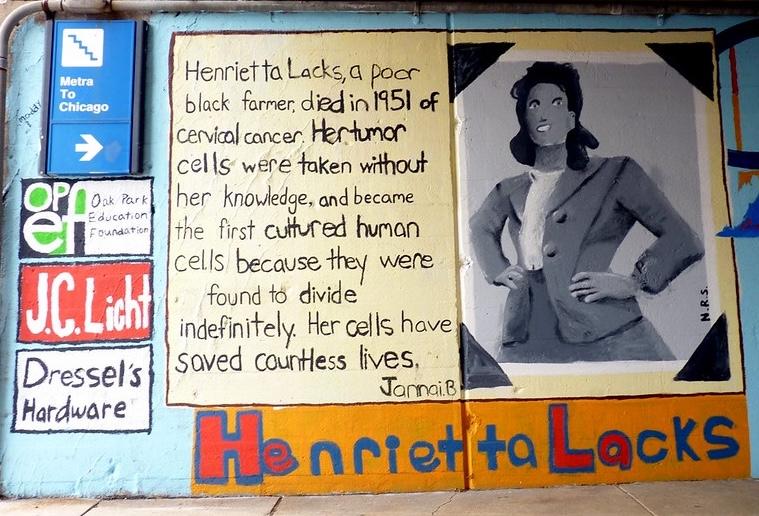
The person behind the acronym HeLa is Henrietta Lacks, a Black woman and mother of five who worked in a tobacco factory. In 1951, at the age of 30, she was diagnosed with cervical cancer and was examined at Johns Hopkins Hospital in Baltimore, Maryland, where her doctor, George Otto Gey, removed tumor tissue without informing her—a common practice at the time. Gey continued to culture these cells, and while Lacks died that same year, her tumor cells continued to grow indefinitely.
Although researchers had long known the origin of the immortal HeLa cell lines, the Lacks family only learned of their existence in 1975. To give a sense of how widely they are used, the biomedical database PubMed lists over 4,000 scientific publications in which the cell line plays a role published in 2022 and 2023 alone. Pharmaceutical companies made a lot of money from the drugs based on research using HeLa, and countless scientists built their careers on experiments with the cell line, but the Lacks family continued to live in poverty and without health insurance.
The collection and commercialization of cells without profit sharing or informed consent from those affected was not unusual in the 1950s. But as Skloot vividly illustrates in her book The Immortal Life of Henrietta Lacks, Lacks’ identity as an African American woman was an important factor in shaping how she and her cells were treated. Lacks had been a patient at Johns Hopkins because it was one of the only hospitals in Baltimore that would treat Black people, and the institution offered free treatment for poor people. However, this “free” treatment came with a cost. According to Skloot, physicians felt entitled to conduct research on patients as “payment” for their treatment.
Because the Lacks family lacked access to education and because the hospital did not readily disclose their use of Henrietta Lacks’ cells, the family did not understand what exactly happened to their mother's cells, even after they were informed. When scientists approached the family in 1975 about taking cells from them to conduct research, Lacks’ husband initially thought his wife was still alive and scientists had locked her in a cell to conduct research on her. It was only through contact with Skloot that the family was able to fully come to terms with what had happened to Henrietta Lacks and demand justice.
Not a problem of the past
In 1964, the World Medical Association adopted the Declaration of Helsinki, which sets out ethical principles such as informed consent when dealing with research subjects. But ethically problematic research practices are by no means limited to the last century, including in the HeLa case. In 2013, a German research team from the European Bioinformatics Institute in Heidelberg made the complete genome of HeLa cells available online using a database of the US National Health Authority (NIH). Although the researchers mentioned Henrietta Lacks in the acknowledgements of the accompanying technical article, they did not deem it necessary to obtain the consent of the Lacks family, whose genetic information was thus also involuntarily published. The family protested, and the NIH agreed to withdraw the publication and to make the HeLa genome sequence available to researchers only after a case review. However, then-NIH head Francis Collins felt it was important to note that the NIH was “responding to an extraordinary situation here, not setting a precedent for research with previously stored, de-identified specimens.” Collins pointed out that the non-identifiability of biospecimens was “increasingly illusory, owing to technological advances.” The case illustrates how the current scientific trend toward Open Access can be problematic when it comes to research with human genetic data: The requirements of many journals and research funders to make all data public in the spirit of scientific cooperation can result in sensitive privacy violations for the test subjects and their families. Indigenous communities have initiated debate about data sovereignty, but there has so far been little acknowledgment of this problem in the life sciences.
Late justice
In 2021, Henrietta Lacks' survivors started to fight for financial justice. They sued the pharmaceutical company Thermo Fisher Scientific, alleging that the company made a conscious decision to commercialize the cells and profit from a racist medical system. According to the lawsuit, there are at least 12 products marketed by Thermo Fisher that contain the HeLa cell line. “The exploitation of Henrietta Lacks represents the unfortunately common struggle experienced by Black people throughout US history. Indeed, Black suffering has fueled innumerable medical progress and profit, without just compensation or recognition," said Ben Crump, the widely known civil rights attorney representing the Lacks family, who previously represented the family of George Floyd.
In August it became known that the Lacks family and Thermo Fisher had agreed to a settlement, but details of the deal were not disclosed. The family has since filed a lawsuit against another company that made a profit from HeLa cells: Ultragenyx Pharmaceutical. According to Crump, the company’s “choice to continue utilizing HeLa cells despite the cell line’s origin and the concrete harm it inflicts on the Lacks family can only be understood as a choice to embrace a legacy of racial injustice embedded in the U.S. research and medical systems.” The Lacks family's efforts could be a model for other cases where tissues from patients were commercialized without their consent. Perhaps the renewed debate about HeLa cells will bring to an end the questionable research practice of using pseudonymization or anonymization to wipe away all thoughts of the individual behind the tissue sample.
Dr. Isabelle Bartram is Program Director at Gen-ethisches Netzwerk (Gen-ethical Network), a Berlin-based nonprofit organization advocating for the responsible use and governance of human genetics. She is a molecular biologist at the University of Freiburg’s Institute of Sociology.